Abstract

Background: Adults with chronic immune thrombocytopenia (ITP) have increased risk of arterial thromboembolism (TE) compared to the general population. Adequate therapy with antiplatelets, anticoagulants or revascularization may be limited by thrombocytopenia and bleeding risk. Few studies have examined the quality of arterial TE management in ITP, and outcomes such as bleeding and cardiovascular deaths.
Aims: To examine acute inpatient management and outcomes of arterial TE in relapsed/refractory ITP.
Methods: This multicentre retrospective cohort study included all chronic ITP patients ≥18 years who received second-line therapy (2012-2020) in the province of Alberta, Canada. Demographics, ITP disease characteristics, traditional vascular risk factors, and history of TE were collected. We also collected ITP-related thrombotic risk factors including splenectomy status, antiphospholipid antibody syndrome (APS), and use of thrombopoietin receptor agonists (TPO-RA) at the time of TE. The incidence rate was calculated by dividing the number of TE events by the person-years of follow-up since ITP diagnosis. For each TE event, we examined the initial and nadir platelet counts, acute ITP-directed therapy, and quality of TE management (antiplatelets, anticoagulants, revascularization) during hospitalization. We assessed outcomes including 30-day mortality, cardiovascular deaths, and bleeding from TE event to last follow-up or death. Research ethics approval was obtained.
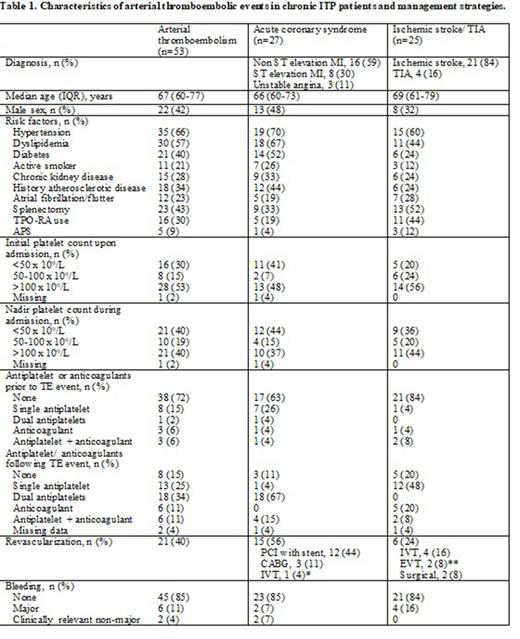
Results: During 2713 person-years of follow-up since ITP diagnosis, 46/329 patients (14%) developed a total of 53 incident arterial TE events, 9 of whom also developed venous thromboembolism. TE events included 27 (51%) acute coronary syndromes (ACS), 25 (47%) ischemic strokes or transient ischemic attacks (TIA), and 1 (2%) acute limb ischemia. The incidence rate of arterial TE was 2.0 (95% CI 1.5-2.6) per 100 person-years. The median age at time of arterial TE was 67 years (IQR 61-77), 22 (42%) were men (Table 1). Risk factors for arterial TE included: history of atherosclerotic disease (18; 34%), 3 or more traditional vascular risk factors (17; 32%), post-splenectomy status (23; 43%), concurrent TPO-RA use (16; 30%), and APS (5; 9%). Most (37; 70%) were not on antiplatelets or anticoagulants at presentation. Of these, 7 had interruption or discontinuation of prior antiplatelets/anticoagulants due to bleeding risk, and subsequently developed ischemic stroke/TIA.
A platelet count <50 x 109/L was observed in 21 (40%) arterial TE events throughout hospitalization. Acute ITP therapies to maintain platelet >50 x 109/L included: IVIG (9/21; 43%), platelet transfusions (7; 33%), TPO-RA (6; 29%), corticosteroids (4; 19%), and rituximab (4; 19%). Of the 27 ACS events, over half (15; 56%) underwent revascularization with either PCI (5 bare metal stents, 6 drug-eluting stents, 1 catheter-directed thrombolysis) or coronary artery bypass graft (3). Patients with platelet count >50 x 109/L showed a non-significant trend towards higher likelihood of revascularization (10/15, 67%) compared to those with platelet count <50 x 109/L (5/11, 45%; P=0.28). Three patients received neither antiplatelets nor revascularization due to severe thrombocytopenia (<30 x 109/L). Of the 25 stroke/TIA events, 6 (24%) underwent revascularization. Antiplatelet or anticoagulants were not offered in 5 cases, mostly due to thrombocytopenia and/or hemorrhagic transformation.
At last follow-up, 26/46 (57%) patients died at a median age of 74 (IQR 64-80) years, from cardiovascular deaths (n=10), other TE (n=2), infection (n=7), bleeding (n=1) and other causes (n=6). The 30-day mortality following TE was 10%. Major bleeding occurred in 6 (11%) individuals, at a median of 18 days (IQR 14-32) after TE.
Conclusion: Patients with chronic ITP receive suboptimal management of arterial TE including a lower likelihood of receiving antiplatelet/anticoagulants or revascularization. With the advent of newer lines of ITP therapies including three TPO-RAs and fostamatinib, aggressive ITP control is critical to avoid withholding antiplatelet/anticoagulants, and to reduce the risk of bleeding, recurrent TE, and cardiovascular deaths.
Disclosures
Wu:Pfizer, Leo Pharma, Servier, BMS-Pfizer: Honoraria. Sun:Sanofi/Sobi, Shire/Takeda: Honoraria.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal